
Chapter 2: Stigma
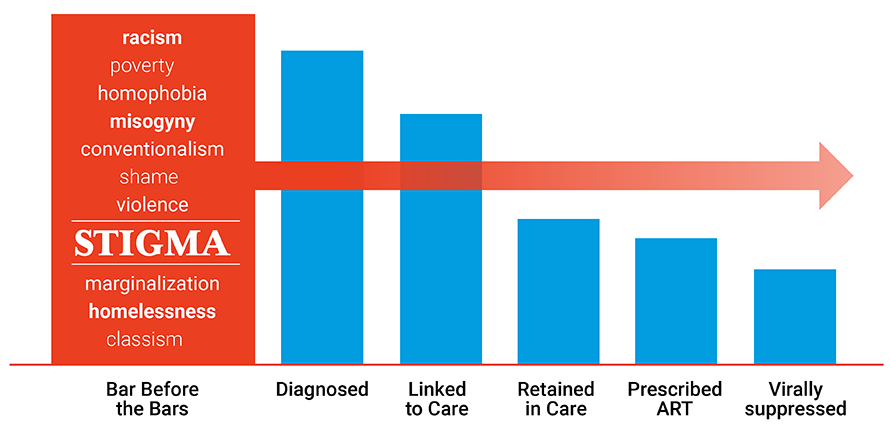
Stigma and epidemics of HIV and hepatitis have long been intertwined. Stigma refers to the social devaluation of people who are different, whether due to conditions that do not affect the majority of a population (e.g., physical handicaps, HIV, mental illness), or more common conditions that affect many or all in a population (e.g., demographic features tied to age, ethnicity, gender). Stigma, in its varying forms, serves to fuel the propagation of HIV and hepatitis, notably within marginalized communities. The complex role stigma plays in poor sexual health outcomes among gay, bisexual, and other men who have sex with men – and the resulting disproportionate rates of HIV and hepatitis among the population – are oftentimes overlooked in the realm of HIV prevention. To effectively respond to the HIV epidemics affecting Black and Latino gay, bisexual, and other men who have sex with men, it is imperative that we address the pervasive stigma related to homosexuality, race, and gender nonconformity.
Our treatment of HIV has advanced. Why hasn’t the stigma changed? | TEDx Vermillion Street
Despite advances in HIV treatment since the beginning of the epidemic, stigma targeted at PLWH remains. This TED Talk explores what it is like to live with HIV, benefitting from medical advancements, but still having to endure stigma on a daily basis. 17 min, 7 sec
Health Department Examples
Alabama
Start Talking Alabama: Alabama’s Stigma Reduction and HIV Awareness Raising Social Media Campaign is a video series that seeks to increase HIV awareness and decrease stigma by sharing prevention, testing, and treatment information, and supporting messages aimed towards young men of color via social media. The “Start Talking Alabama” campaign was developed as an offshoot of the Centers for Disease Control and Prevention (CDC) "Start Talking Stop HIV" campaign.
Wisconsin
Wisconsin Department of Health Services’ program to Increase Leadership Diversity in the HIV Workforce: Rates of HIV are unacceptably high and increasing among young Black gay and bisexual men and transgender women. Increasing workforce diversity, particularly at the leadership level, is crucial to addressing the disparate impact of the epidemic on these populations. The Wisconsin Health Leaders Fellowship is a one year leadership development program designed to increase the number of leadership positions held by people of color, particularly men who have sex with men (MSM) of color, in organizations providing HIV services in Milwaukee, Wisconsin. Fellows come from five local agencies which have committed to the program and to supporting staff to participate as fellows. The fellowship is coordinated and supported by the Wisconsin AIDS/HIV Program at the Wisconsin Division of Public Health.
Key Resources
Addressing Stigma: A Blueprint for Improving HIV/STD Prevention and Care Outcomes for Black & Latino Gay Men | NASTAD 17 pages
Conversations on Stigma: A Resource Guide for Health Departments *Anticipated release date: June 2019*
Additional Resources
Let’s Stop HIV Together Stigma Fact Sheet | CDC 2 pages
Ending the Epidemics: The Role of the Affordable Care Act & Medicaid | NASTAD 2 pages
HIV – how to fight an epidemic of bad laws | TEDx Summit 15 min, 22 sec
How to overcome our biases? Walk boldly toward them | TEDx Beacon Street 17 min, 50 sec
Check Your Understanding
What implicit biases do you hold that may hinder your service to people living with HIV and/or HCV?
We all have implicit biases, despite our good intentions. We must work to discover what our biases are and work to ensure they do not hinder our work. Implicit biases could include prejudices to groups of people based upon their gender identity, ethnic background, geographic location, history of drug use, history of sex work, etc. We can acknowledge that people may be different than ourselves, but must also believe that all people are valued, regardless of background and life choices.
What policies or practices do your health department employ that may perform a disservice to the very populations you intend to serve?
Like implicit biases, you may find that your health department operates under policies or practices that do not serve priority populations. Consider whether your workforce and planning councils mirror the demographic background of the communities you serve. Are there policies that hinder specific populations from accessing services (e.g., sobriety restrictions on curative HCV treatment)? Do providers’ practices align with desired outcomes (e.g., routine HIV testing and prescribing PrEP)? Consider what type of ongoing education and/or training is necessary to identify and rectify negative policies and practices.
How do you hold funded providers accountable for ensuring their services are inclusive and culturally responsive?
A recurring concern from communities is that providers’ discriminatory actions hinder people from seeking out testing and treatment services. Cultural responsiveness training should be ongoing, and involved all levels of staff (e.g., front desk staff, mid-levels, providers, etc.). Please see “Additional Resources” on this page to access examples of training opportunities.