Impact of Trauma and Opportunities for Healing Across the HIV Continuum
Past and current traumatic experiences can have impacts along the HIV continuum and can contribute to an individual’s health outcomes; however, opportunities for healing across the continuum are plentiful.
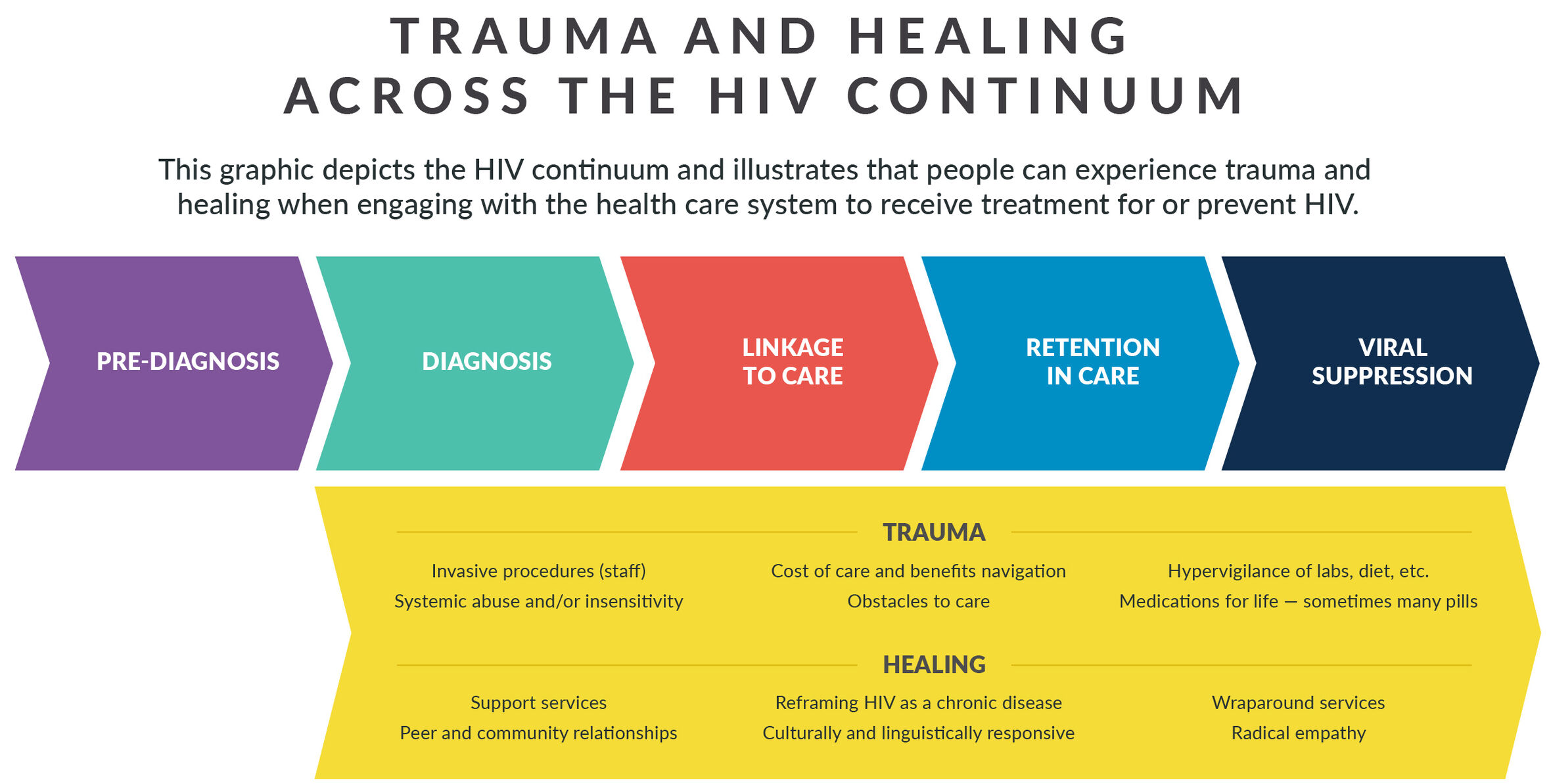
Past traumatic experiences can lead to coping behaviors that increase a person’s risk for HIV, such as sex without the use of prevention tools or barriers and chaotic drug use. A status-neutral approach incorporates a trauma-informed approach to HIV testing and offers linkage to prevention services for people who test negative. Prevention services, including use of Pre-exposure prophylaxis (PrEP), should be trauma-informed and include culturally and linguistically responsive testing, information, and referral services.
Pre-Diagnosis Reflection Questions
Use the following reflection questions for the "Pre-Diagnosis" stage of the HIV continuum to delve deeper into an understanding of the experience an individual may go through and how you can best support them along the way.
- How does your division/bureau engage individuals pre-diagnosis?
- How does your division/bureau implement a status neutral approach?
The impact of receiving an HIV diagnosis can be exacerbated by the:
- Method of delivery (e.g., by letter, phone call, or partner disclosure)
- Person delivering the diagnosis (e.g., use of stigmatizing language, discriminatory practices or treatment, or lack of training)
- Health of the person receiving the diagnosis (e.g., the person is experiencing a life-threatening illness at time of diagnosis)
- Timeliness of the diagnosis (e.g., lab results taking longer than expected or are inconclusive)
- Other related fears (e.g., disclosures, threat of intimate partner violence).
Avoidance of stressful experiences is common among people who have experienced trauma and may contribute to delayed testing and diagnosis.
Alternatively, streamlining of administrative processes provide opportunities for healing. For example, as noted by the TIA Toolkit Advisory Panel (TAP), offering rapid start to medications, support services, or peer services on the same day as diagnosis can create a sense of comfort and control for the client. Suggestions offered by the TIA TAP include framing of HIV as a chronic disease, like diabetes or high blood pressure, which can normalize the stress of receiving a HIV diagnosis. Ensuring results and referrals are provided by a culturally and linguistically responsive provider is imperative.
Diagnosis Reflection Questions
Use the following reflection questions for the "Diagnosis" stage of the HIV continuum to delve deeper into an understanding of the experience an individual may go through and how you can best support them along the way.
- What training is provided to those who will be giving the diagnosis?
- Is there an opportunity to engage the individual in holistic care or support (i.e., providing for their physical, mental, spiritual, and social needs )?If so, what would that look like?
- Are T cells and CD4 count explained to the individual? How about undetectable = untransmittable? Do they leave your facility with the understanding that HIV is similar to any other chronic disease?
The experience of linking to care may be traumatic due to invasive medical procedures, insensitive providers, cost of care, and navigation of health and medication benefits. Required disease investigation services may be intrusive and raise questions about privacy and confidentiality for individuals just diagnosed. Other obstacles to care include housing, transportation, adequate treatment for mental health and substance use disorder, health literacy, documentation requirements, and language and cultural barriers. By contrast, low barrier access to services, provision of culturally and linguistically responsive, and peer-delivered services can result in effective linkages to care. Radical empathy for those newly diagnosed but not yet ready to engage in care is paramount. Consider using NASTAD’s Healing-Centered Considerations for Program Intake and Psychosocial Assessments tool to identify ways to incorporate more healing-centered questions and processes as you link newly diagnosed individuals into care.
Linkage to Care Reflection Questions
Use the following reflection questions for the "Linkage to Care" stage of the HIV continuum to delve deeper into an understanding of the experience an individual may go through and how you can best support them along the way.
- How do you assess an individual's level of comfort and safety?
- How do you collaborate to determine next steps post-diagnosis and connection to care?
- Are the organizations you connect individuals to agencies that you would go to yourself?
People who have experienced trauma often have difficulty staying in care. Despite the best intentions of providers, HIV medical care and support services can be re-traumatizing. For example, providers may be late, rushed, or distracted during an appointment; use overly complicated or redundant forms, procedures, or policies; expect perfect adherence or immediate behavior change; and ignore client’s perspectives about treatment or services. Often, behaviors such as taking medication erratically or not attending appointments can be linked back to an individual’s history of trauma. Considering the impact of trauma may help providers empathize with clients to better understand behaviors and enable more effective communication and relationship-building that can lead to better outcomes for both clients and staff (e.g., job satisfaction and connection to clients). For some individuals, engagement in the Ryan White HIV/AIDS Program (RWHAP) may offer opportunities for services, such as dental care or housing support, which may be a higher priority for individuals than taking HIV medications. The TIA TAP noted that because healing can mean different things to different people, it is important to provide wraparound services without requirement or expectation for engagement in HIV medical care.
Retention in Care Reflection Questions
Use the following reflection questions for the "Retention in Care" stage of the HIV continuum to delve deeper into an understanding of the experience an individual may go through and how you can best support them along the way.
- How do you assess factors that contribute to keeping individuals retained in care?
- What is your course of action when you receive poor feedback about an individual’s experience with a specific provider or provider agency?
For those individuals engaged in care, resilience is positively associated with treatment adherence and undetectable viral load. For example, one study among HIV positive women found a positive correlation between resilience and medication adherence. Conversely, trauma can be associated with a variety of poor health outcomes, including treatment adherence issues. It is important to consider that viral suppression may not be a goal for an individual; perhaps housing or social and emotional support are their priorities. Although we know viral suppression is key to the physical health of a person with HIV and their community, as well as to the RWHAP, the TIA TAP emphasized the importance of prioritizing the way that individual defines health and wellness and to meet them where they are.
Viral Suppression Reflection Questions
Use the following reflection questions for the "Viral Suppression" stage of the HIV continuum to delve deeper into an understanding of the experience an individual may go through and how you can best support them along the way.
- What is the language utilized when discussing the importance of viral suppression with an individual? Does the individual even understand the term?
- How do you assess contributing factors leading to viral suppression?