
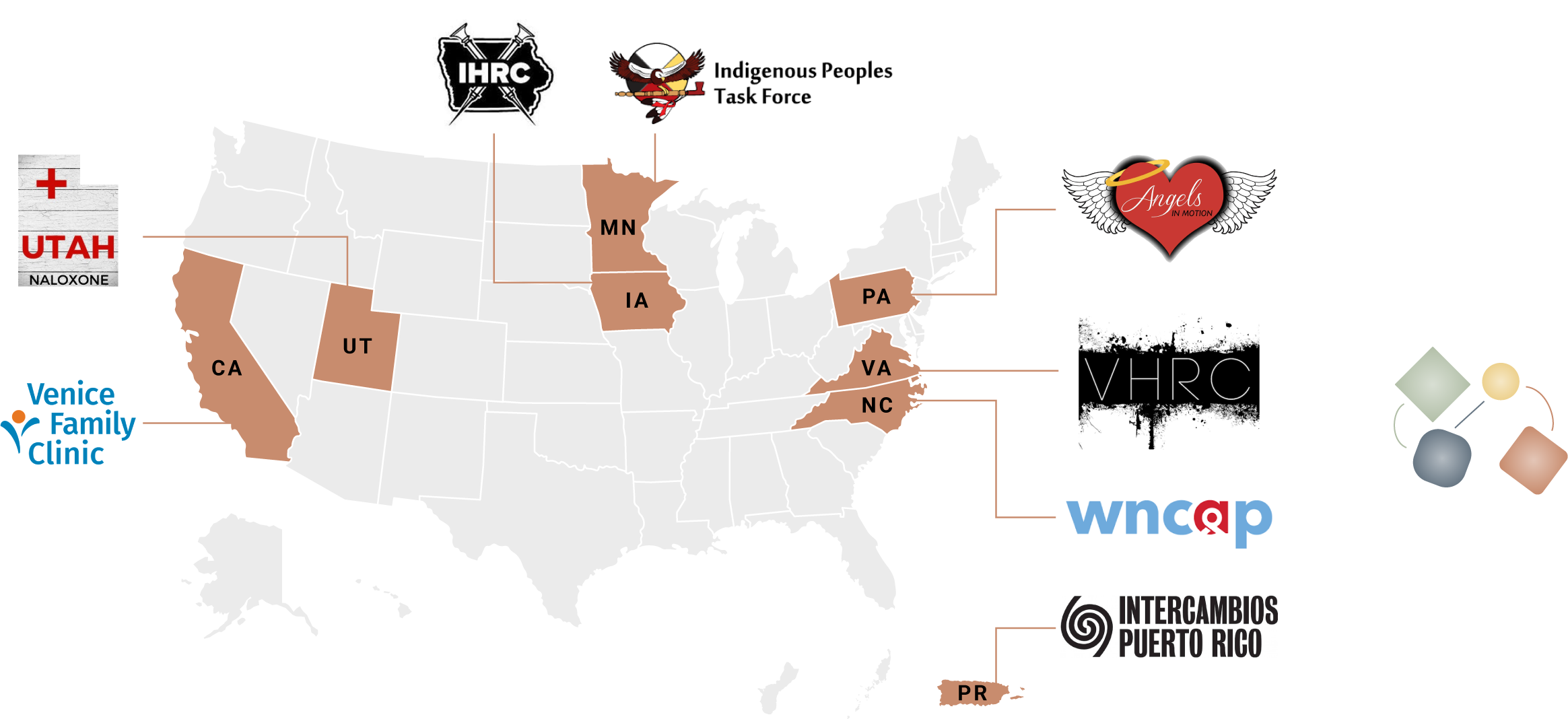
Project Sites
Across the eight project sites and over two years of funding, more than 1,151 participants engaged in patient navigation services that offered connections to a wide variety of medical and social services.
All sites designated at least one full-time staff member to the project, who was responsible for participant engagement, care planning and navigation, and case management and documentation. The patient navigator(s) at each site worked with NASTAD and AU TA providers on program planning, implementation, and data collection. Regular engagement with patient navigators allowed TA providers to facilitate sharing of promising strategies and approaches between project sites and receive real-time feedback that informed the course of the project. Group check-in and TA calls became important opportunities for peer engagement and problem-solving, especially following the onset of the COVID-19 pandemic early in the project.
Selecting Programs
When selecting programs for participation, NASTAD looked for variation in structure, setting, and capacity. Unlike a pilot project that tests the viability of an intervention, this demonstration project sought to learn from implementation and operation and to create usable guidance for existing and emergent navigation services. The concept of patient navigation is well-established for many areas of care, and SSPs often offer some level of resource navigation in their core services, but little formal guidance for comprehensive SSP-based patient navigation existed prior to the project—guidance on, for example, appropriate budget amounts for effective programs, staffing recommendations, and the establishment of accountable relationships with external service providers.
Participating programs ranged in size and operating budget, geographic setting and urbanity, service populations, comprehensiveness of existing services, and organizational structure, representing the breadth of current harm reduction programs and the ongoing uptake of harm reduction approaches by other types of medical and social service providers.
Sites were divided into groups, beginning implementation in March 2020, July 2020, and August 2020. This was intended to allow some programs, by request, more time to prepare and hire staff and to encourage peer TA and shared learning between sites at different project stages. NASTAD held an initial kick-off training in Washington, DC, with the first five programs in February 2020 and a virtual second kick-off during Summer 2020— given the onset of COVID-19 and limitations on travel.
Timeline

Cohort 1
March 2020 launch:
- Utah Naloxone, a harm reduction program run in collaboration with the University of Utah Medical Center, based in Salt Lake City, UT;
- Intercambios Puerto Rico, a non-governmental medical and social services organization serving a predominantly rural community in eastern Puerto Rico, based in Fajardo, PR;
- Indigenous Peoples Task Force, a long-standing AIDS service organization led by and primarily serving the local urban Native community and surrounding reservations, based in Minneapolis, MN;
- Iowa Harm Reduction Coalition, a grassroots statewide harm reduction service and advocacy organization, based in Des Moines, IA;
- Western North Carolina AIDS Project, a long-standing AIDS service organization working locally and in several rural counties, based in Asheville, NC;
Cohort 2
July 2020 launch:
- Common Ground at Venice Family Clinic, a community-based SSP now operated by a federally qualified health center, based in Los Angeles, CA;
- Virginia Harm Reduction Coalition, a community-led statewide harm reduction service organization, based in Roanoke, VA;
Cohort 3
August 2020 launch:
- Angels in Motion, an emerging community response and harm reduction program, based in Philadelphia, PA.