Virginia Harm Reduction Coalition
As a patient navigator…never give up even when it gets hard. It’s amazing to see participants get back on the right track, after you provide them with resources, the basics, things we all need and deserve. Seeing this progress is phenomenal and rewarding for everyone involved.
Highlights:
- Building trust and collaboration with other agencies, particularly the local health department, the Housing Assistance Team, and other medical providers (including within academic institutions), is crucial to ensuring access to comprehensive services for PWUD.
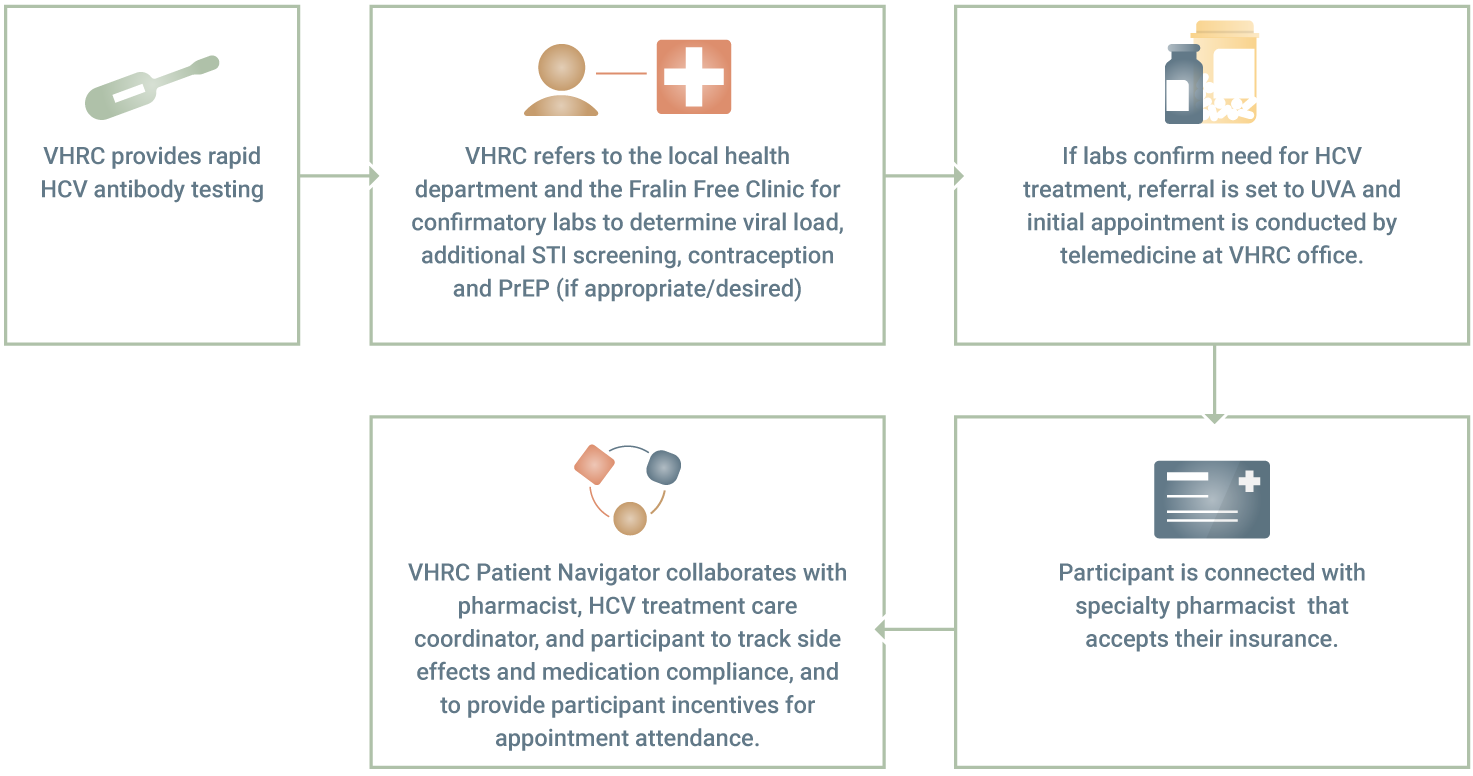
- VHRC facilitated access to HCV treatment for SSP participants by coordinating care between multiple agencies and providers, arranging for participants to attend telemedicine appointments at the VHRC office, and providing incentives.
- Stigma against PWUD in healthcare and social service settings is persistent. Although the presence of a patient navigator was able to mitigate the impact in some circumstances, PWUD frequently face mistreatment and lack of compassionate, trauma-informed care.
- VHRC, like many other SSPs, experienced community-level stigma and discrimination in the form of negative media portrayals and refusal to lease office space to the program. For VHRC, this caused program instability, a temporary switch to exclusively mobile services, and disruptions in navigation for PWUD.
Program Overview
Virginia Harm Reduction Coalition (VHRC) is a nonprofit peer-run organization located in Roanoke, Virginia. VHRC’s mission is to improve the health of the community it serves by developing and implementing evidence-based solutions to address the adverse effects of drug use. They address health inequities faced by PWUD by providing outreach to marginalized, stigmatized, and criminalized populations, advocating for health policies that address their specific needs, and collaborating with other agencies to effectively meet those needs.
Through the project, VHRC helped participants gain access to governmental assistance programs. They also conducted HCV testing and assisted with connections to HCV treatment via telemedicine. Through their referral and navigation efforts, participants were able to connect with SUD treatment providers and secure permanent or temporary housing. VHRC prioritized working with participants to identify goals based on their unique needs, and participants have reported that patient navigation has filled a gap that was previously missing from VHRC. According to VHRC’s patient navigator, “they are able to come into a space, where they feel comfortable and loved, and let go of all the weight and burden that follows them everywhere they go looking for help anywhere else within the community.” The navigator built strong relationships with participants, and they frequently visited to check-in, share progress updates, and provide feedback on the results of previous referrals.
Project Impact
VHRC was proactive in building partnerships with local service providers to address participants’ needs and facilitate access to comprehensive services, and continued to collaborate with local health departments, medical care providers, community service boards, and housing providers throughout the project and beyond. VHRC built an intentional partnership with the Roanoke Housing Assistance Team for support around navigating systemic barriers to housing access. In addition to finding creative solutions to secure temporary or permanent housing within the current system, VHRC worked towards systemic change by joining local coalitions and working groups to share the barriers faced by participants (particularly PWUD and survivors of intimate partner violence) and advocate for policy change.
VHRC established a network of relationships with other agencies to coordinate access to Hepatitis C treatment, including the state’s Hepatitis C Education and Patient Connection (HEPC) program, the University of Virginia (UVA), the Roanoke City Health Department, and the Fralin Free Clinic. By hosting telehealth appointments at VHRC offices, participants could experience a quiet, familiar, and emotionally safe space in which to engage with providers. VHRC secured additional funding to provide participant incentives for each appointment and to purchase phones for those in need to ensure continuous access to telehealth appointments. They also worked with a specialty pharmacist at UVA to send participant medication directly to VHRC’s office and schedule phone calls with participants using the VHRC office phone. This flexibility, plus VHRC’s ability to provide participant incentives, proved to be incredibly effective at engaging participants in HCV treatment. During the first three months of implementation, 12 participants completed their HCV labs and 9 participants attended HCV telehealth appointments, receiving prescriptions for HCV treatment medication. One participant had initiated their medication and the 8 remaining participants with prescriptions were anticipated to initiate their treatment shortly.
During Year 2 of the project, VHRC entered into a partnership with the Roanoke City Health Department to host vaccination clinics during outreach, aimed at increasing participant access to immunizations against COVID-19, hepatitis A, and hepatitis B. Not only were the clinics successful in providing vaccinations to participants, but these events also provided opportunities for VHRC to educate health department staff on the complex needs and lived experiences of PWUD.
Project Challenges
VHRC faced a number of challenges throughout the project period, including the COVID-19 pandemic, stigma and discrimination against PWUD, lack of available housing, and staff shortages. Shelter in place orders and limited in-person contact due to COVID-19 impacted access to services throughout the state. To reduce COVID-19 transmission, many providers restricted new client admissions, resulting in longer wait lists and more difficulty accessing SUD treatment, HCV care, and other critical services.
Stigma and discrimination against PWUD continued to be a significant issue across community providers, impacting VHRC’s ability to effectively link participants to other services. Participants were less likely to continue services if faced with poor treatment and stigma during appointments, and even in instances when the navigator accompanied participants to appointments, mistreatment by healthcare staff still occurred. This revealed a significant lack of access to trauma-informed and compassionate care outside of VHRC. Access to safe, supportive, and permanent housing continued to be a critical need among participants throughout the project, and PWUD were frequently excluded from shelters and housing assistance. Sobriety requirements in order to access HCV treatment were common, and VHRC struggled to find low-barrier and non-judgmental HCV care for participants during Year 1.
Community-level discrimination of participants also presented unique challenges. Local businesses near VHRC’s office began to cite complaints and publish media reports about empty naloxone boxes, graffiti, and feeling unsafe – all of which appeared to be thinly veiled stigma against program participants. As a result, VHRC was not given the option to renew their lease and was forced to close their office in June 2021. In the search for a new office space, VHRC experienced an unwillingness among businesses, neighbors, and landlords to lease office space to an SSP. A new office was finally secured six months later in January 2022 and mobile services continued in the interim.
Naloxone shortages and newly imposed monthly limits on the amount of naloxone programs could receive from the state also impacted harm reduction organizations across the state and imposed an additional burden on VHRC staff to secure naloxone from other sources. Staff turnover, including the departure of the patient navigator, also impacted VHRC’s ability to ensure accurate data collection and reporting at times, and with a steady increase of SSP participants, the program became understaffed. During Year 2, a new Executive Director was hired and the previous patient navigator returned to VHRC, allowing the program to regain stability and expand services.
Patient Engagement and Navigation
During the project period, VHRC documented over 1,200 participant/patient navigator touch points, including 64 referrals for SUD treatment, 137 enrollments in supplemental nutrition assistance and Medicaid, and 135 navigation encounters related to hepatitis C (rapid/confirmatory testing, lab work, and referrals to treatment). HCV treatment became more readily available to participants through partnerships with the Roanoke City Health Department, UVA, and the state’s HEPC program during Year 2. Through a partnership with the Roanoke Housing Assistance Team, VHRC provided 89 referrals to participants for temporary or permanent housing. VHRC held vaccination clinics in collaboration with the Roanoke City and Alleghany Health Districts where participants were provided immunization against COVID-19 (180 individuals), hepatitis A (195 individuals), and hepatitis B (133 individuals).
The table below demonstrates the various touchpoints that VHRC had with participants and services provided throughout the project period.
VHRC Patient Navigation Encounters (July 2020 – June 2022)
Total Number of Participant/Patient Navigator touchpoints - 1228
|
Service |
Number of Encounters |
|
Benefit Enrollments (SNAP and health insurance) |
137 |
|
SUD Treatment Referrals |
64 |
|
HCV Navigation Interactions |
135 |
|
Housing Referrals |
89 |
|
ID Assistances |
20 |
|
Domestic Violence Case Management & Referrals |
68 |
|
COVID-19 Vaccination |
180 |
|
Hepatitis A Vaccination |
195 |
|
Hepatitis B Vaccination |
133 |
|
Referrals to Other Medical Services |
302 |
Case Study
VHRC’s patient navigator had been working with a pregnant woman in her 20s who lived in a local women's shelter. The participant had a history of methamphetamine use, had children who had already been removed from her care, and was at risk of losing custody of her new baby if she tested positive for amphetamines. The patient navigator was a source of emotional support for this participant as she struggled with cravings, finding employment, the arrest of her abuser, and attempts to regain custody of her children.
With the help of the patient navigator, the participant was able to secure permanent housing, overcome transportation barriers to her new job as a CNA, and receive regular prenatal care for her new baby. The participant delivered her daughter on January 7, 2021. The participant subsequently lost custody of her daughter due to non-compliance with her recovery plan, which was created by the Department of Social Services without input from the participant or the patient navigator. However, at the time writing the participant is working full-time and has not used methamphetamine or heroin in 13 months. She is currently undergoing Hepatitis C treatment with VHRC’s assistance, and the navigator meets with her regularly to support her recovery path.
This case demonstrates the importance of the relationship that patient navigators develop with SSP participants. The navigator continued to provide support and helped the participant remain focused on her short and long-term goals, despite significant challenges. The navigation process is rarely linear and must remain responsive to the changing life circumstances of each participant. Patient navigation support has assisted the participant in achieving the goals of finding employment and permanent housing. Meeting these immediate needs created a foundation to pursue the longer-term goals of undergoing HCV treatment, stopping drug use, and working to regain custody of her children.
A successful patient navigator is compassionate and understanding of the client’s perspective and allows them to take control of their own lives and assists however the client deems necessary.
Takeaways and Next Steps
Dedicated funding and support for patient navigation services allowed VHRC to provide participant-centered, trauma-informed case management that meets participants where they are. The rapid growth and interest in these services fully demonstrates the ongoing need for patient navigation with dedicated funding and support to expand such services. VHRC aims to continue providing navigation services and seek out funding opportunities to expand staff capacity to provide even more participants with vital resources. As social and financial support for harm reduction continues to grow, VHRC advises programs to leverage funds to treat and support the whole individual, rather than focusing solely on drug use. By meeting the diverse needs of participants, VHRC was able to remove barriers to healthier use and empower participants to take control of their lives and health.
Each client's success is their success. Although we assist them by providing patient navigation, they take it upon themselves to undergo this path to improve their quality of life.