Phases of Emergency and Service Disruption Preparedness
Phases of Emergency Preparedness
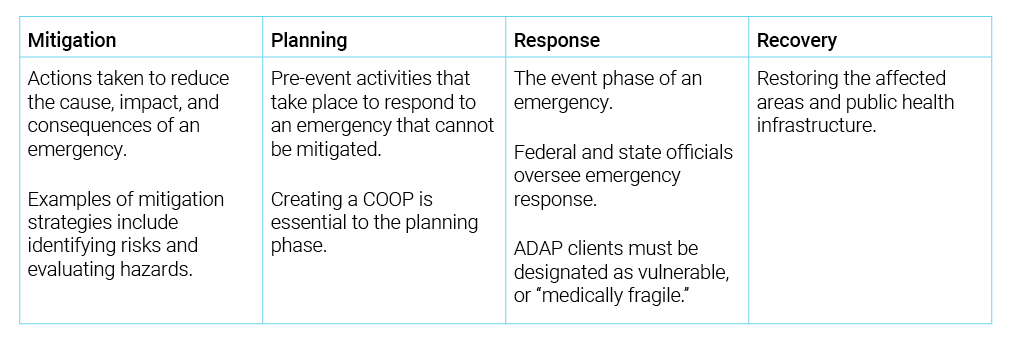
There are four critical and interconnected phases of emergency and service disruption preparedness: mitigation, planning, response, and recovery. Focused effort during the planning phase will help ensure the response and recovery phases occur in a timely and efficient manner. A brief description of each phase is listed below:
This document will focus on the second phase, planning, the most critical phase of emergency preparedness. Please note, emergency preparedness plans should consider local factors, and be revisited and revised regularly.
Planning Phase of Emergency and Service Disruption Preparedness
There are six major components of the Planning Phase for Emergency and Service Disruption Preparedness. Following each section is a brief listing of considerations and associated resources.
1. Conduct a Risk Assessment
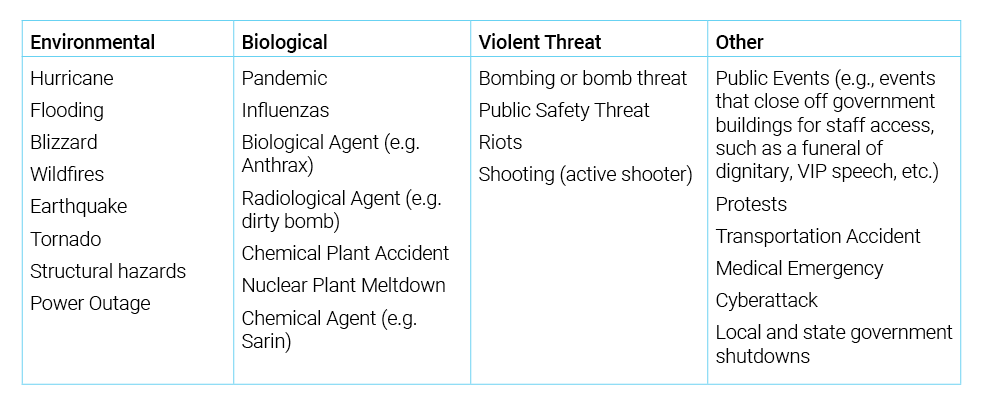
Conduct a risk assessment: To create a strong plan, ADAP administrators should determine what types of hazards pose the greatest risks for ADAP disruptions in their state and regional areas.
Risk assessment considerations:
Identify the hazard(s) most likely to impact your program’s operations
Considerations:
-
Consider the length of time of disruption. Some may be for a few hours or a few days; some may be weeks or months.
-
Determine program vulnerabilities. Since ADAP service delivery is generally dependent on local (e.g., health department), statewide (e.g., network pharmacies, service providers), and national (e.g., pharmacy benefit managers, insurance benefit managers) system components that can be impacted by emergencies and other hazards, these should be risk assessment considerations.
-
Develop preliminary contingency plans or back-up response to address vulnerabilities.
-
Prioritize Primary Mission Essential Functions of the ADAP.
Resources:
2. Identify Key Partnerships
Identify Key Partnerships: Solidify working relationships and agreements with key organizations and stakeholders before an emergency or service disruption.
Considerations:
- Ensure all relevant ADAP system components are included in planning:
- Pharmacy wholesaler(s) and other distributors
- Pharmacy Benefits Manager (PBM)
- Pharmacy provider network
- State pharmacy
- Insurance Benefit Manager (IBM)
- Non-traditional partners for emergency assistance for program clients
- Strategic National Stockpile (SNS)
- Drug manufacturer patient assistance programs (PAPs)
- Engage all HIV service providers in planning:
- In-state partnerships, such as Ryan White HIV/AIDS Program Part A, B, C and/or D recipients and other HIV service providers
- Interstate partnerships (e.g., communicating with bordering states about possible collaboration/Emergency Management Assistance Compacts [EMACs; see below] regarding ADAP coverage in emergency situations)
- Federal partners
- Engage/involve clients and community leaders to prepare for a coordinated effort and to elicit feedback related to planning efforts.
3. Assess Differences in Evacuation vs. Shelter-in-Place
Assess differences in evacuation vs. shelter-in-place: ADAP program administrators should determine how the plan needs to address any differences between an evacuation and shelter-in-place situations.
Evacuation vs. Shelter-in-Place Considerations:
Evacuation: Organized, phased, and supervised withdrawal, dispersal, or removal of civilians from dangerous or potentially dangerous areas, and their reception and care in safe areas.
Shelter-in-Place: The use of a structure to temporarily separate individuals from a hazard or threat.
- For evacuation:
- Plan for medication distribution by ensuring an up-to-date registry of clients with accurate medication history can be accessed by pre-determined Point of Distribution (POD) sites and/or other states.
- Allow for pharmacy network exceptions for individuals who many not have access to their regular pharmacy or pharmacy within the ADAP’s current network.
- Consider establishing an EMAC with neighboring states to address ADAP needs of emergency evacuees.
- For shelter-in-place:
- Include a plan to deliver medications to client homes in the event of shelter-in-place requirement.
- For both evacuation and shelter-in-place situations:
- Include policies that allow for early refills and/or dispensing limit overrides (e.g., 60- or 90-day fill allowances) when potential emergencies are anticipated.
- Streamline and/or create virtual program recertification and renewal processes.
- Plan for continued monitoring and tracking through hotlines.
- Distribute communication flyers through local social service organizations, AIDS service organizations, or FEMA Disaster Recovery Centers.
- Provide HIV education and materials to state and federal “special needs” or “medically fragile” shelters in advance of an emergency.
Resources:
4. Develop an Emergency Plan for Staff (individuals and families)
Develop an emergency plan for staff (individuals and families).
Considerations:
1. Consider and discuss the emergencies most likely to affect your community and/or state operations.
2. Complete a comprehensive emergency plan for evacuation and facilitate evacuation exercises with staff.
- Determine how emergency alert/warning systems and signals can be monitored, and when emergency plans should be activated.
-
Review the organization’s overall emergency plans with staff; make sure they are familiar with roles and confirm they can carry out assigned responsibilities.
-
Facilitate exercises to practice the plan and identify any gaps or deficiencies in the plan.
3. Collect and assemble three supply kits (home, work, and vehicle).
Resources:
5. Assist Clients with Emergency Planning
Assist clients with emergency planning.
Evacuation vs. Shelter-in-Place Considerations:
1. For evacuation:
- Before an emergency, assist clients in identifying and planning for their specific needs during an emergency.
- Provide clients with emergency planning resources (e.g., printed one-page guide). Information may be included as a medication insert with prescriptions and/or staff can share information at standing planning meetings, with client groups, or during program certification and recertification processes.
- Educate clients to:
-
Have a current prescription for all medications and keep at least a 14-day supply of medications on hand.
-
Keep a list of all medications and emergency contacts.
-
Keep at least three days of non-perishable food items that meet the energy, protein, fat, and micronutrient requirements for medication and health needs.
-
Store at least one gallon of water per person per day. As a minimum, have three days’ worth of water on hand.
-
2. For shelter-in-place:
- Educate clients to have the following additional supplies:
-
Alternative telephone service (cordless or wireless phone if possible).
-
Plastic sheeting, duct tape, and scissors to cover doors or windows, mirrors, etc.
-
A radio with extra batteries.
-
Toilet tissue, hygiene products, trash bags, and a bucket (which can be used for a toilet).
-
Resources:
6. Create and Maintain a Continuity of Operations Plan (COOP)
Create and Maintain a Continuity of Operations Plan (COOP).
As reviewed in the next section, the creation, implementation, and maintenance of a COOP is integral to operationalizing the necessary measures to maintain or restore the ADAP functions that provide clients access to medications during an emergency situation. The COOP should be based on the specific risks and hazards identified for the ADAP and shared with all stakeholders. All parties should know the role they have in implementing the COOP.