HIV & Housing
Housing is the greatest unmet need for people living with HIV (PLWH) and one of the strongest predictors of health outcomes. Across the U.S., upwards of 70% of all PLWH report experiencing homelessness or housing instability. On any given day, three to ten percent of all homeless persons are HIV positive.
The rates of HIV infection are up to 16x higher for people who are homeless than those stably housed. For PLWH who are homeless, on average, entrance into care is delayed for six months. Additionally, homeless men who have sex with men (MSM) are 15x more likely to delay HIV testing than stably housed MSM.
Homelessness and HIV/AIDS have a complex relationship, presenting many more challenges as providers work to improve disease outcomes for clients. Lack of housing is often an overarching barrier, with many other housing-related issues, like nutrition security, impacting stability. When housing is addressed clients have improved viral loads, medication adherence, mental health, and overall better quality of life.
Washington State
Since 1981, when the first case of AIDS was diagnosed in Washington state, more than 20,000 people have been diagnosed with HIV. Over 6,700 people have died as a result of HIV.
As of 2015, more than 12,500 people were reported to be living with HIV in Washington state. However, there has been a decrease in the number of new HIV cases over the past five years (2011-2015); roughly 470 new cases are diagnosed each year.
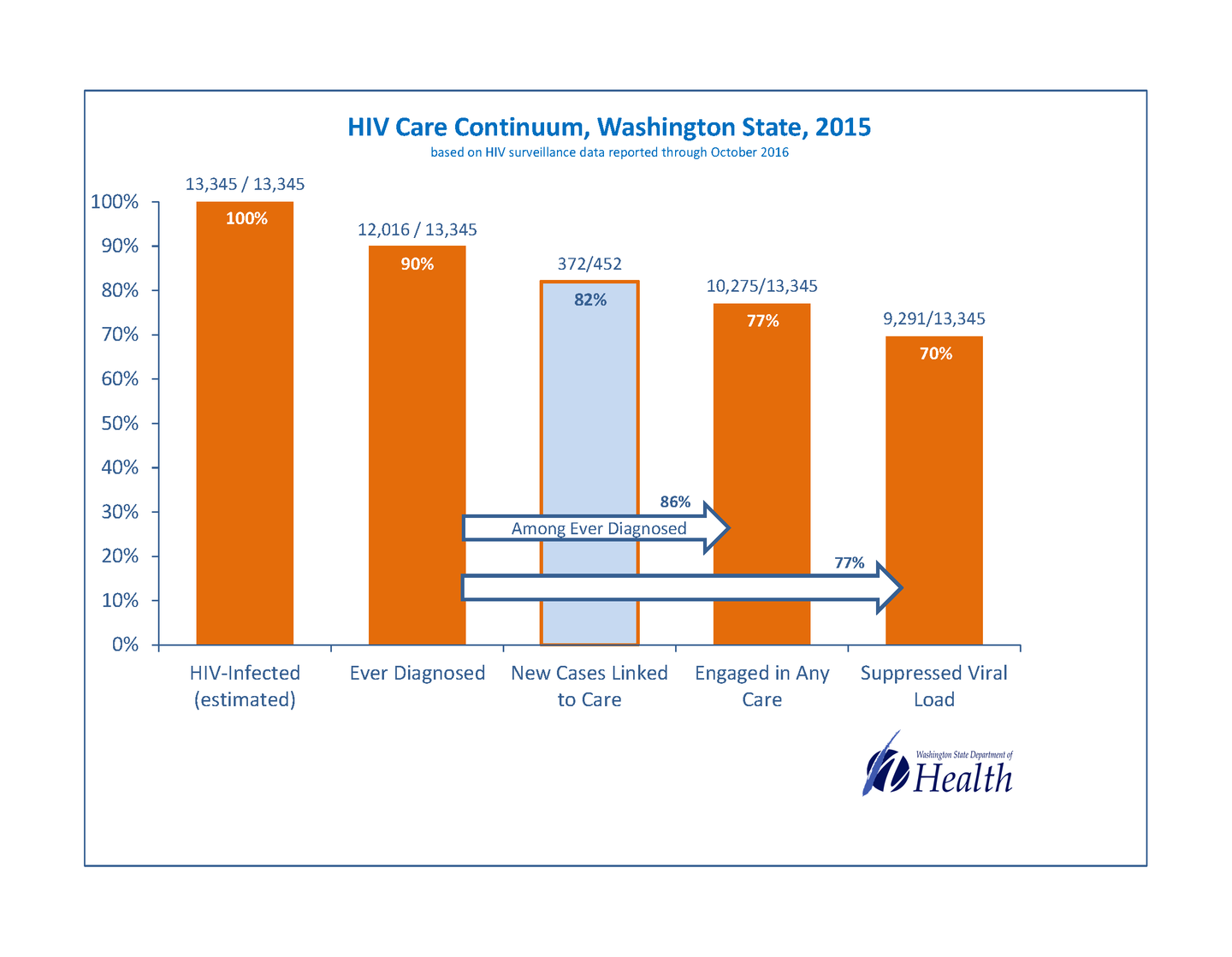
Through a collaboration of government agencies, community organizations, and educational and research institutions, Washington state created The End AIDS Washington Initiative. This collaboration works together to improve the quality of life for those living with HIV by 2020. As part of the goals, the initiative looks reduce the number of new HIV infections by 50%, get to 80% suppressed viral load across its continuum, decrease HIV mortality to 25%, and reduce health disparities. Included in this initiative The Washington State Department of Health, which funds HIV core medical and support services, included addressing housing, exclusive of the Seattle & King County region.

On any given night throughout the state of Washington, an estimated 20,827 (2016) people are experiencing homelessness/unstable housing. Of that total, 8,466 (40.7%) people are unsheltered, living on the streets, or in places unfit for human habitation. The majority of those experiencing homelessness are individuals, but there are an estimated 6,927 people in families with children and 1,307 unaccompanied youth who are experiencing homelessness.
Seattle/King County has the largest concentrated population of people in Washington experiencing homelessness (10,730). Nationally, as of 2016, Seattle/King County ranked third as a major city Continuum of Care with the largest number of homeless people. With rapid population increases, in November 2015, Mayor Ed Murray (Seattle) and King County Executive, Dow Constantine declared a state of emergency in the number of people who are homeless in Seattle/King County. Despite the many programs and services available to people who are homeless, or at risk of homelessness, the number of individuals/families who need additional support outweighed the capacity of the city/county. By declaring a state of emergency, the city and county hope to bring increased funding and support to the organizations that are addressing housing services.


Eliminating homelessness is a major focus of many community partners and health departments. HIV service providers are involved in a series of activities designed to best understand and tackle this critical issue. Efforts around this need are taking place at the Washington State Department of Health and collaborative agencies.
Housing and other non-medical services are vital to the success of clients. When clients feel safe and supported, their self-efficacy to manage their disease increases.
Emergency declarations are associated with natural disasters, but the persistent and growing phenomenon of homelessness – here and nationwide – is a human-made crisis just as devastating to thousands as a flood or fire. We call on the federal and state governments to take action, including shouldering more responsibility for affordable housing, mental health treatment, and addiction services.
Program Implementation
In 2015, the Washington State Department of Health reached out to consumers and providers via site visits and needs assessments to gather information on community/client needs. Through this feedback and national research, the need for housing stability and housing-related services emerged. The Department of Health recognized that stable housing is critical to achieving other life domain stability, including ongoing medical retention and consistent viral suppression, as well as achievement of overall improved health outcomes.
In response to national research and the feedback, the Washington State Department of Health added direct subsidy of housing/housing-related expenses to the menu of fundable services available to their sub-recipients providing case management services to people living with HIV (PLWH). The Department of Health allowed a considerable amount of autonomy to the sub-recipients around the dispensation of housing service funds.
In 2016, the Department of Health began a quiet campaign to encourage sub-recipients to provide housing services. Like viral non-suppression, disengagement with medical care, and recent justice involvement, unstable housing became a reason to categorize a client as moderate- or high- need.
Simultaneously, the Department of Health held conversations with Public Health Seattle & King County, which manages the Ryan White Part A funded services Transitional Grant Area (TGA). Through these conversations, the Department of Health assessed how the TGA approached housing needs in their region and engaged with HOPWA. Understanding their methodology, process, and program structure was crucial to creating a solid partnership and further developing the Department of Health’s housing program.
For new contracts in 2017 the Department of Health prioritized housing for sub-recipients. The Department of Health’s staff developed regional housing status reports to identify utilization, gaps in care, and community needs. The status reports formed the foundation for providing support to sub-recipients as they developed housing programs that fit the needs of their communities.
As of the end of 2016, the total number of unduplicated clients who accessed the housing subsidies was 122. Population viral suppression changed from 70% virally suppressed (unstably housed) to 90% virally suppressed (within in 6 months of achieving stable housing). An increase in case management retention of stably housed over unstably housed has also been observed. As the Department of Health moves forward, they intend to continue reaching out to the community with questions and for guidance, to truly meet the needs as they define, understand, and experience them.
Program Structure

What housing services are available through the program?
The Department of Health funds sub-recipients to provide housing services. Sub-recipients make payments directly to the vendor. Direct payment non-voucher financial assistance is available for established rentals, deposits, transitional units, emergency motel, emergency shelter, essential housing-related utilities, and application costs related to acquiring safe housing. All agencies currently funded under this category are additionally funded to provide Case Management.
All beneficiaries of housing subsidies through the Department of Health must participate in the creation and execution of a Housing Service Plan. The client's Housing Service Plan draws from information gathered through the initial intake, a comprehensive assessment, ongoing case notes, individualized case management service plans, and communicated information from other team members, providers, and the client.
What housing-related services are provided in the program?
Clients receiving assistance for housing needs are additionally eligible for other Department of Health-funded core medical and supportive services. These can include, case management, nutrition services, transportation services, mental health and substance disorder prevention, and treatment services, early intervention services (EIS) services, psychosocial support, and outreach.


What data were used, if any, to inform program structure?
Data referenced throughout the process includes the Medical Monitoring Project (MMP), 2014 and 2015 WA RSR Data, and Public Health Seattle & King County HIV Provider Survey/Consumer Needs Assessment.
Funding Structure
What funding sources contribute to the program?
All funding comes from Rebate Dollars secondarily derived from their ADAP program.
Are there any benefit restrictions?
There is a household income cap of 400% Federal Poverty Level (FPL) placed on Housing Services. This matches Washington's current cap on ADAP, as well as, all support services, other than case management, for which there is no cap. Clients are eligible for housing assistance and subsidies for no more than 24 total lifetime months.
Lessons Learned
What are the biggest barriers clients experience while accessing services or in housing placement?
Structural barriers can often create many obstacles for the clients. One of the most confronted is insufficient housing stock that is safe, affordable, healthy, and fit for human habitation. Among many, some considerations when looking for suitable housing include: landlord discrimination and unit accommodation, access to transportation, sidewalk accessibility, low drug or crime activity neighborhoods, access to groceries, or distance from medical providers.
As for client-related barriers, this includes: poor or no credit/rental history, non-traditional citizenship status, income level, untreated mental health or substance use issues, or criminal history,
These barriers foster frustrations, distrust, and an aversion in clients to continue interaction with these structures and organizations. This ultimately can negatively impact a client's success in securing stable housing and maintaining positive health.
Outcomes and Future Goals
The Department of Health currently measures program success by monitoring viral suppression rates pre- and post- housing subsidization, rates of retention in medical care, and case management retention rates. Moving forward, the Department of Health will measure success by beneficiary retention in stable housing during and post subsidization, and overall population housing stability. The Department of Health is adding Quality of Life questions related to housing to its health survey. They will disseminate this survey to consumers via their attached case management organizations.
To aid in consistent collection of housing-related data, inclusive of both process and outcomes, the Department of Health is revising CAREWare. They are standardizing all fields and services and adding a housing-specific custom tab.
Further, the Department of Health is currently considering adding "housing stability" as a global measure of performance in 2017 and setting targets for overall housing stability. Specifically for those PLWH disproportionately affected by oppressive, inequitable institutionalized systems, inclusive of race, gender identity, nativity, age, and geography.
Housing models previously piloted either by Washington State Department of Health or by Public Health Seattle & King County are planning to be implemented. These include a Medical Motel Model of housing and a Master-Lease Housing Program.
Finally, the Department of Health is considering how to involve their affected communities in meaningful and empowered ways around assessing housing needs, understanding the impact of housing status on HIV-specific outcomes and overall health, and recognizing the impact of policies/programs related to housing. This will be important to conceptualize the best next steps and to create and implement a model of shared leadership with their affected communities.
Acknowledgments
Washington State Department of Health
- Richard Aleshire, HIV Client Services Program Manager
- Karen Robinson, HIV Client Services Community Programs Supervisor
- Sarah Fanucci, Statewide Case Management Coordinator
Pierce County AIDS Foundation (PCAF)
- Chris Barrans, Client Services Director
- Deborah Green, Client Assistance Program Manager
- John Watson, Client
Field Studio Films
- Hannah Ayers
- Lance Warren
NASTAD
- Kristina Santana, Senior Manager, Prevention
- Natalie Cramer, Deputy Executive Director
- Angela Johnson, Director, Prevention
- Jillian Casey, Senior Manager, Prevention
