Tier 1 Grantees
Overview
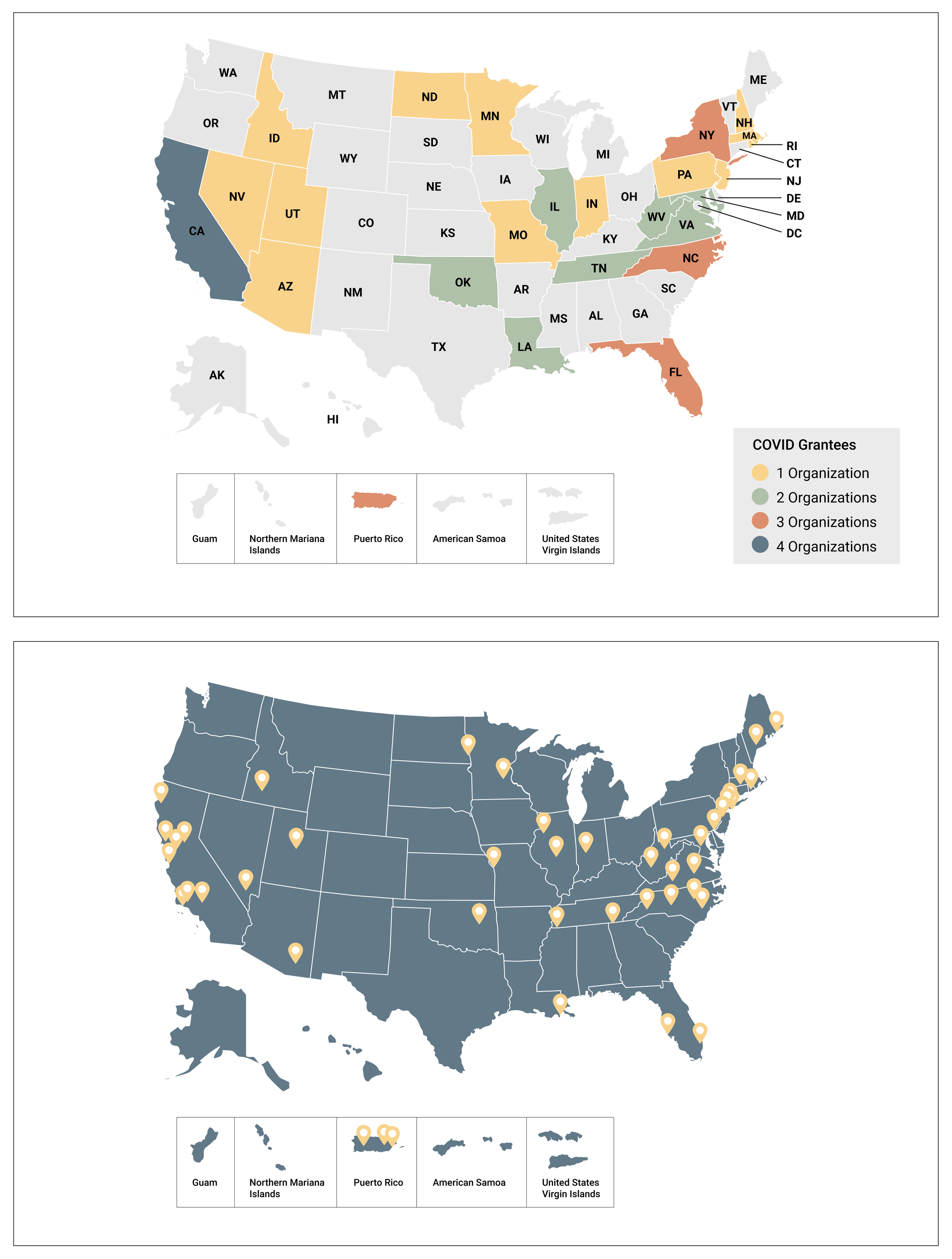
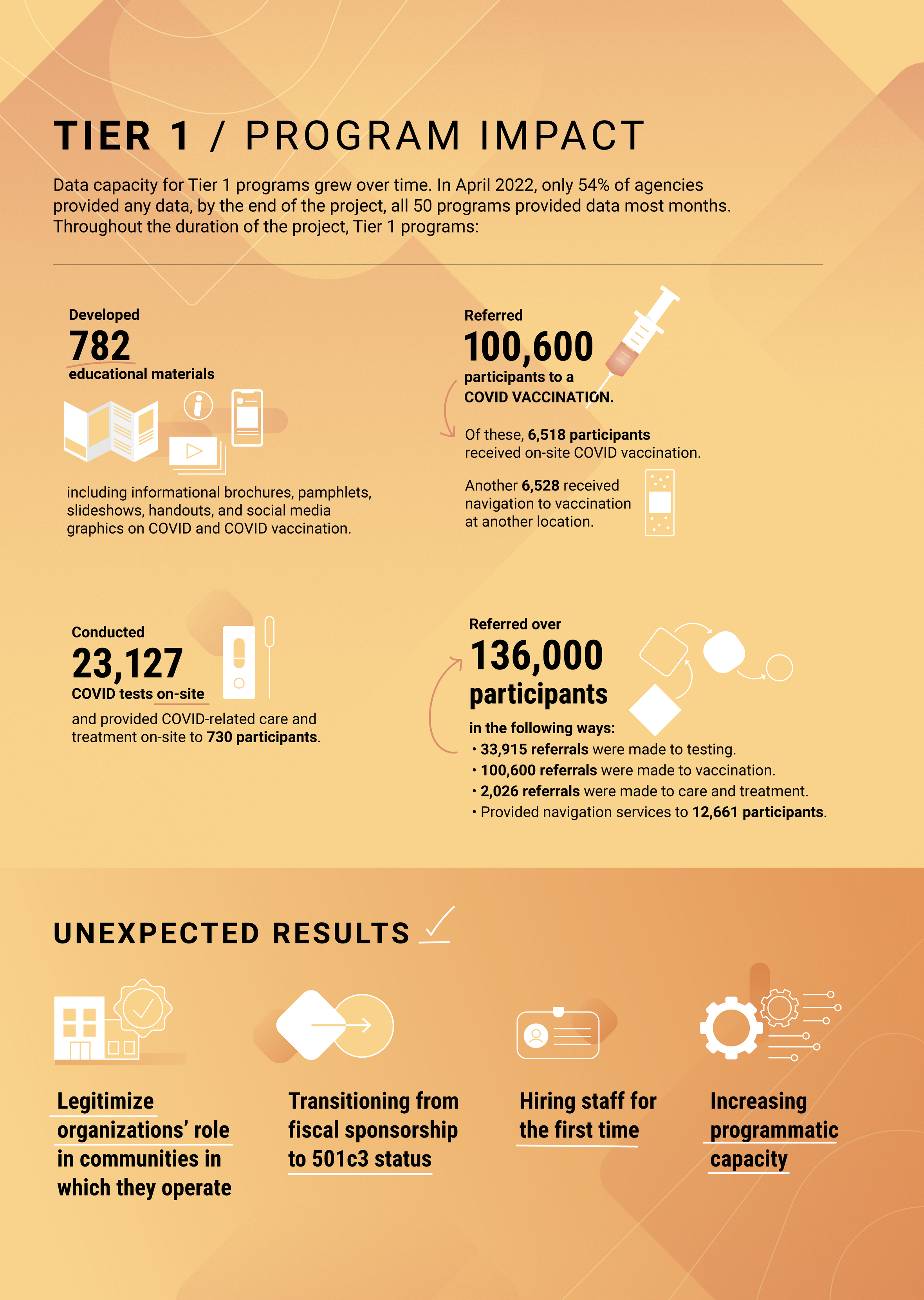
Tier 1 grantees represent our low-threshold Tier of funding. Fifty (50) syringe services programs (SSPs) were selected with each to receive a total award of $100,000 each. Tier 1 were low barrier grants 'approved by CDC project staff, nearly unprecedented in terms of funding for SSPs. The 50 grantees primarily focused on core services, education, risk reduction counseling, and/or referral or navigation to COVID-19 vaccination/testing/care, with on-site services optional. AIDS United (AU) managed Tier 1 activities and oversaw support and technical assistance. Grantees worked across 25 states and Puerto Rico. One New York-based program operates a mail-based model which provides services nationally to under resourced areas of the country, and one Florida-based program operates statewide.
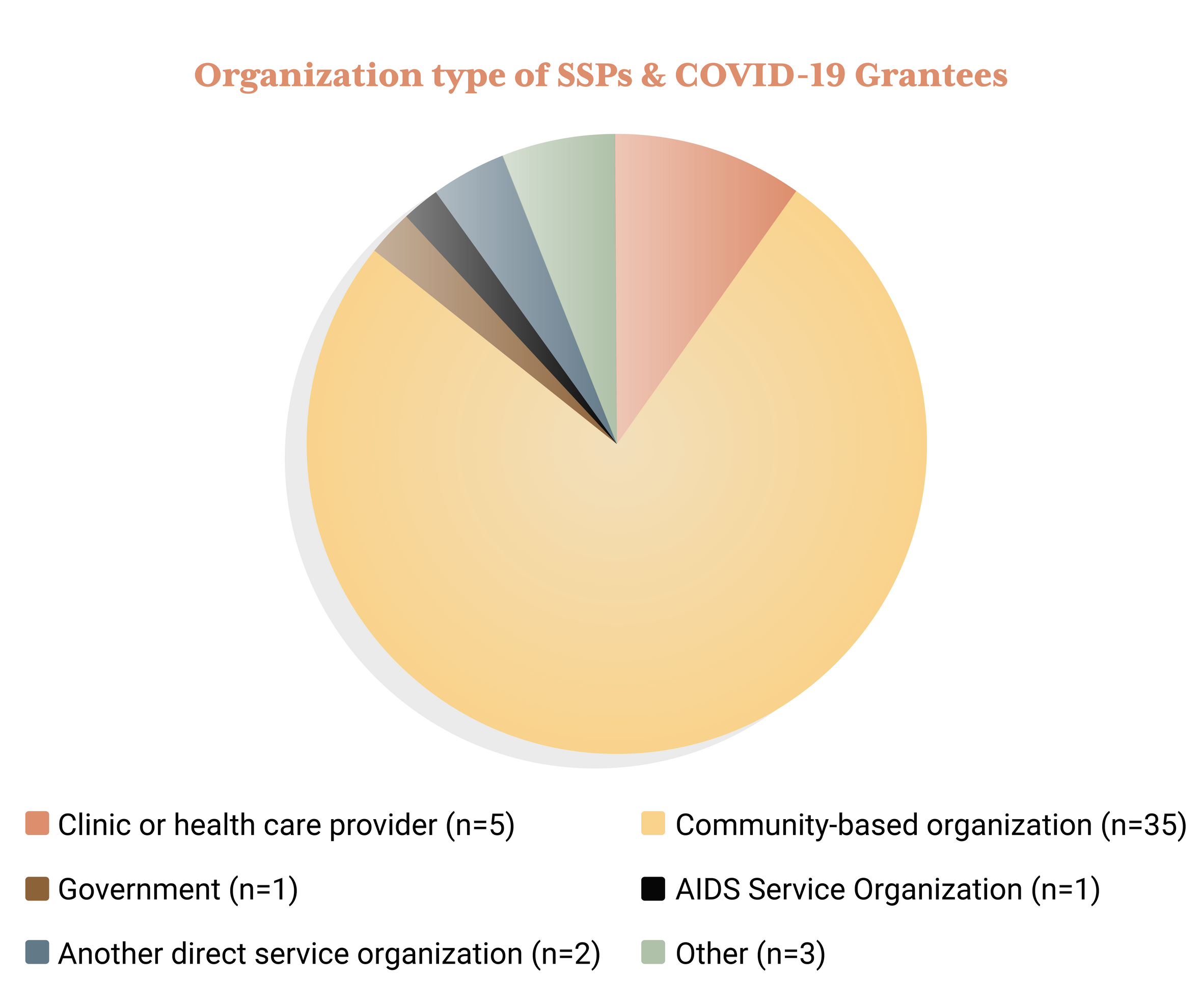
Grantee Maps
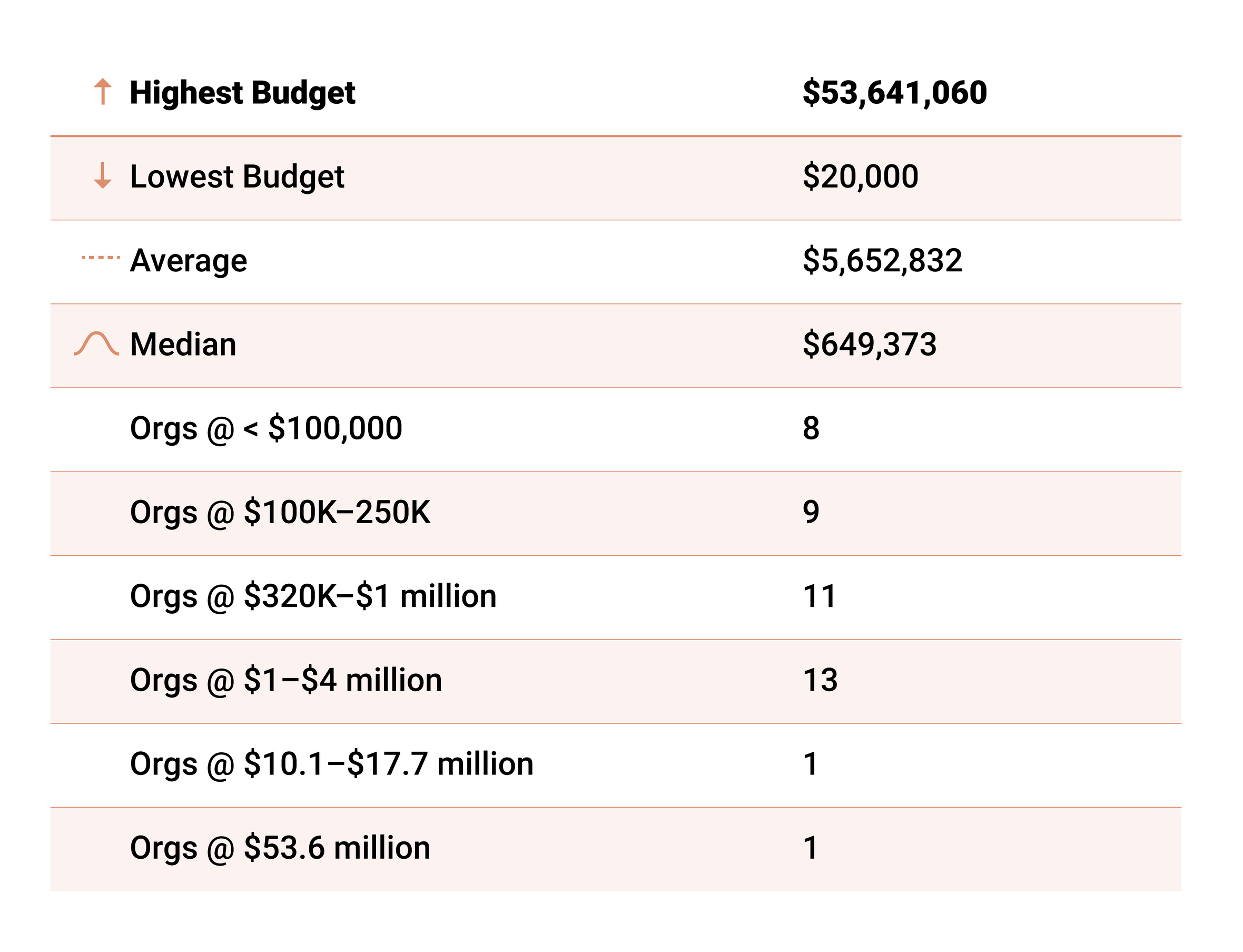
Organizational Types
The majority of grantees fell within four organizational types, with community-based organizations being the most common. There were also clinics/healthcare providers, a public health department, and an AIDS Service Organization (ASO) represented, as well as a handful of service organizations that did not identify with any of these categories.
Annual Operating Budget
There is significant variability in the operating budget size of selected grantees, with the spread provided in the table below. Bear in mind that while total organizational budgets may have high overall budgets, this rarely represents the syringe services program budget, with even large, well-funded organizations housing smaller or under-resourced SSPs.
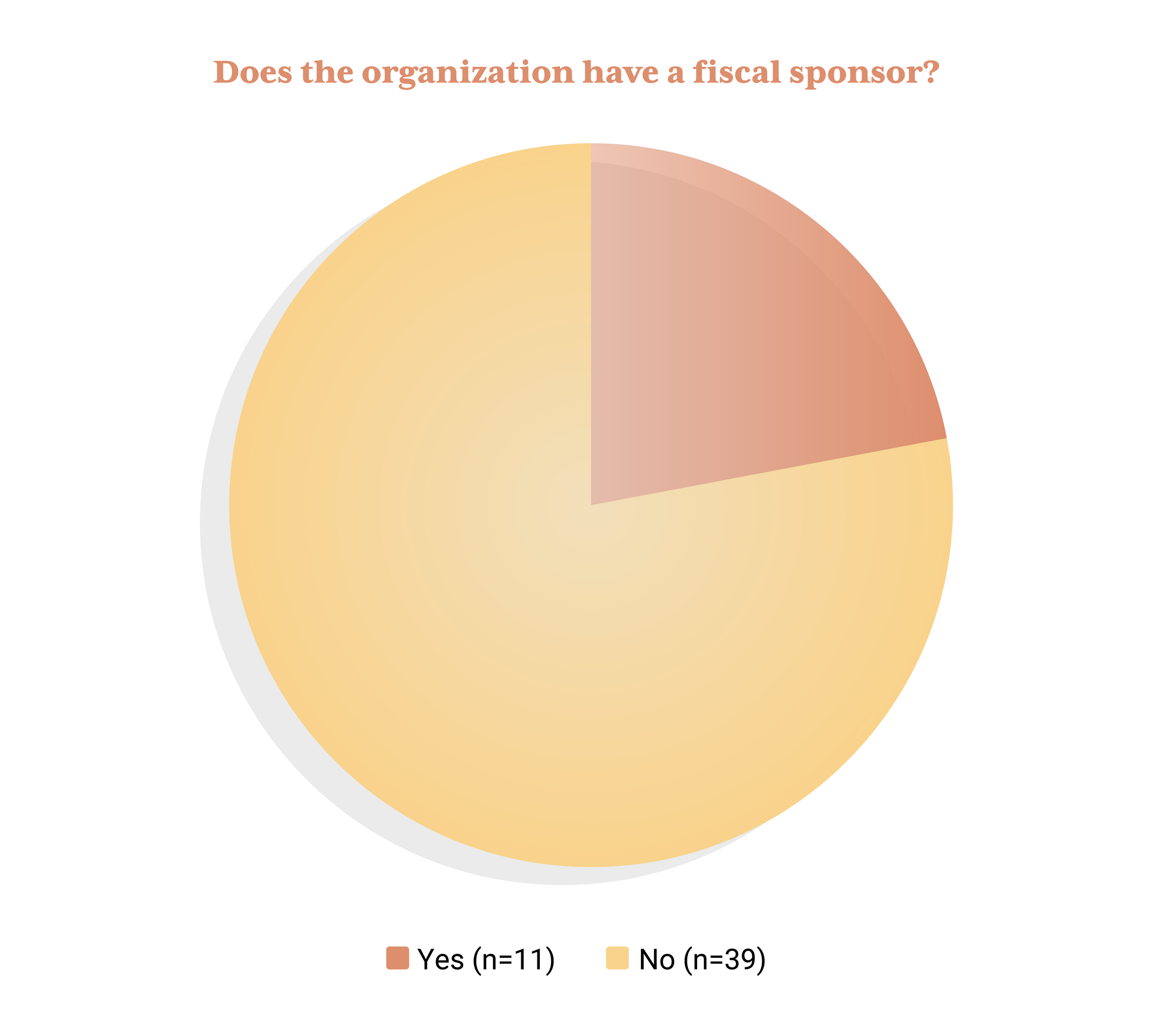
Fiscally-Sponsored Projects
Of the 50 selected grantees, 22% are fiscally-sponsored projects. Low-barrier grants like this opportunity are especially critical, as these organizations typically do not have the capacity or infrastructure to compete for large, federal grants and often represent smaller, grassroots, community-based SSPs in comparison to their 501c3 counterparts.
Self-Identified PWUD-led SSPs
With stigma against people who use drugs still widespread, especially in “professional” spaces, it can be challenging for an organization to openly identify as being led by people who actively use drugs, even among syringe services programs. SSPs are often not accustomed to this quality being prioritized and valued by funders, particularly when associated with the federal government. However, several SSP grantees openly self-identify as being led by people who use drugs (PWUD). Many more also prioritize the leadership of those with “lived or living experience,” which could include prior or current drug use and often feels like a safer way to identify. Among those self-identified PWUD-led SSPs are:
- Harm Reduction Coalition of Santa Cruz (CA)
- HRH413 (MA)
- Humboldt Area Center for Harm Reduction (CA)
- Indiana Recovery Alliance (IN)
- New Jersey Harm Reduction Coalition (NJ)
- NEXT Harm Reduction (NY/National)
- Rebel Recovery Florida (FL)
- Trystereo/New Orleans Harm Reduction Network (LA)
- West Oakland Punks with Lunch (CA)
Overview of Services
A detailed overview of Tier 1 projects is available in the Tier 1 Proposed Project Summary.
Successes and Challenges
This section delves into the successes, challenges, and lessons learned from the Tier 1 programs. These aspects provide valuable insights into best practices and future improvements. It is important to note there was no way to accurately depict the richness and totality of the learnings and experiences, the following represents highlights and common themes from participating programs.
Successes
- Integrating COVID-19, influenza, monkeypox (MPX), and Hepatitis A and B vaccination outreach into existing program models demonstrated peer outreach models are critical to providing COVID-19 education and services and “One stop shop” models are preferred. COVID-19 facilitated participant acceptance of additional adult vaccines and further bolstered community recognition of SSPs as vaccine providers.
- Utilizing incentives for vaccination outreach: Grantees made the distinction between the usefulness of incentives with participants firmly against vaccination, which was largely ineffective, and those who weren’t sure. Incentives were effective in reaching those SSP participants who had not yet made up their minds about COVID vaccination.
- Expansion into new service areas and communities was supported via extended vaccination services, including hepatitis A &B, flu, and MPOX vaccines. Programs also reported that throughout this grant, they’ve been able to expand their services to new locations, such as new towns, counties, and neighborhoods. For some programs, this has also facilitated engagement among new populations as well, including sex workers and LGBTQ+ communities who hadn’t been accessing services before.
- Increased uptake in healthcare services among participants: Grantees utilized a myriad of tactics to address the diversity of need of their clients; ranging from distributing educational materials about COVID-19 to working with participants through vaccine hesitancy by offering both individual and group risk reduction sessions. By providing vaccination and other health-related services on-site (such as wound care and MOUD), participants have been more willing to receive connections to care.
Challenges
- Vaccine Hesitancy: It was noted that even for participants who were not fully against vaccination, obtaining a COVID vaccine was not very high on their priority list. Multiple grantees stated that some participants were so deeply entrenched in anti-COVID vaccination views that they were not sure they could persuade them through education attempts, but kept trying for those participants regardless.
- Hiring and staff retention: One Tier 1 grantee explained the general challenge underlying hiring people with lived and current experience of substance use, as transportation and other logistical challenges create barriers to steady full-time employment. “We prefer people with not only lived experience, but current use experience. We don't have a problem recruiting people who are active users. Having said that, it's not an easy job, right? It's not easy to maneuver.”
- COVID fatigue & burnout among staff and participants had widespread impacts across the cohort. Not only did it create staffing shortages, posing a challenge for continued engagement and program capability, but as critical elements of the frontline, staff were challenged to balance their personal and familial health and wellness with caring for and supporting participants. Similarly, participants also struggled to navigate shifting messaging, fluctuating access to resources, vaccine hesitancy, and stigma amid the intertwined epidemics of HIV, viral hepatitis, and drug use.
- Mixed messaging and changing guidelines around COVID-19 were difficult to navigate and were further exacerbated by the winding down of COVID-19 specific health services. Grantees noted resources or attention shifting away from COVID in the US, irrespective of COVID rates, just as their programming was ramping up. Another Tier 1 grantee noted losing their agency’s onsite vaccine provider because that provider no longer had the staff to prioritize COVID vaccination. Highlighting frustrations with seeing public resources and attention shift away from COVID as their agencies were resourced to provide education and vaccine.
- Limited geographic access to COVID-19 resources and services in rural regions. A Facente survey of Tier 1 demonstrated the geography of an area was clearly related to the accessibility of the SSP, with people in urban areas having more access to SSP services regardless of whether they had a car; though rural programs were more likely to serve participants from multiple counties and/or states. Results also showed SSPs in Medicaid expanded states are more likely to have access to vaccines than those in states without Medicaid expansion further underscoring the impact of a disjointed patchwork of resources on a historically underfunded space.
- Decreasing access to COVID-19 resources: Qualitative data indicate bureaucratic processes around acquiring and delivering vaccine pose significant barriers to provision of services in SSPs and other specialized settings where vulnerable populations are already engaged. This begs the question of to what extent the federal government is willing to support models of expanded vaccine access, which will necessitate reduction of administrative burdens.
- Lack of housing access and gentrification issues had big impacts, though presentation varied across the cohort. Grantees noted increasing encampment sweeps, inclement weather, transportation, unfavorable legislation or ordinances, and NIMBYism (Not in My Backyard) amongst the myriad of issues which disrupted services and increased hurdles for participants.
Lessons Learned
- It is OK and often necessary to adjust project goals and pivot strategies to increase participant engagement and access to services. To be responsive in a fast-paced and ever-changing environment, programs must start with flexibility in mind and build processes and protocols that can flex as challenges emerge and participant needs change.
- Establishing trusting relationships with participants is critical to providing COVID-19 services. Actively listening to participants’ experiences and feedback is key to responsive program design. Bundling services offers increased opportunity for engagement in the target intervention, while still prioritizing participant needs
- Providing COVID services and personal protective equipment (PPE) alongside other services is a great way to engage with folks. Furthermore, offering an array of COVID supplies and services like masks, hand sanitizer, and rapid tests is a concrete way to recognize client differences and preferences that provides anchor points for deeper relationships and higher quality of care.
- Vaccine hesitancy and mistrust is deep-rooted and common but can be reduced. As programs began to explore and deconstruct the drivers of vaccine hesitancy among participants it became clear they were widespread and diverse. By focusing on non-judgmental, non-coercive provision of services and resources, grantees were able to unlock the barriers that hindered many of their participants from vaccination, as well as connect them to additional systems and services they may not accessed otherwise.
- The development of incentives for vaccination services has been helpful to engage with people and proved a powerful motivator. In program design, grantees were mindful about acknowledging existing power imbalances and intentionally concerned with ethics and coercion, resulting in a wide array of creative setups across the cohort.
- Flexibility in service provision is crucial to making services realistically accessible. As the COVID-19 pandemic moved through converging phases, grantees had to take the lead on shifting messaging and services as community needs and guidance changed. This also meant adopting the highest–risk messages, ones that provided the most protection to participants but possibly contradicted inconsistent guidance from jurisdictions, health departments, and the CDC. Grantees changed schedules, delivery methods, and engagement approaches to meet their participants' real needs.
- Fixed costs contracts were specifically chosen for Tier 1 to reduce administrative burden. From a program administration perspective, these contract types were more manageable for grantees and served as a concrete extension of trust, not often afforded to programs of this type and size. We learned some teams preferred the sense of stability rather than risk administrative challenges in tier 2, even if their proposed projects qualified and were appropriate.